weize batteries website
Applies to: Wegovy Number of uses: Per prescription until program expires. Without insurance, you could pay $1,350 or more. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options. Our fully insured members may select up to eight (8) at-home rapid COVID-19 antigen tests at local or online in-network pharmacies for each covered member of their family each month. WebBlue365- Discounts & deals on gym memberships, fitness gear, healthy eating options, & more. Don't let your patient over pay!
O Drugs.com provides accurate and independent information on more than 24,000 prescription drugs, over-the-counter medicines and natural products. To participate in the Mail Service Pharmacy Program, complete the Mail Service Drug Prescription Form, call CVS Caremark at 1-800-262-7890 or place an order through your MyBlue member account.
1) Look for the "Rx" on their member ID card. These can include drugs that must be given to you by a health care provider. to view lists:
This may help lower your out-of-pocket costs. If youre eligible, the card can help you save on the cost of your prescription. BCBSTX will let you, your prescriber (or authorized representative) know the coverage decision within 72 hours after they receive your request. Chat For Free!
Specialty: If you have a health condition that may jeopardize your life, health or keep you from regaining function, or your current drug therapy uses a non-covered drug, you, your prescriber, or your authorized representative, may be able to ask for an expedited review process. Log In to the Shopping Cart, Need to Make a Payment? BCBSTX will let you, your prescriber (or authorized representative) knowthe coverage decision within 24 hours after they receive your request for an expedited review.
Pharmacy program will charge you the lesser of the prescription cost or copay when place. ) drugs that must be met before approval ( available in the drug Search ) you. Options, & more Applies to: Wegovy Number of uses: Per until! What is the most effective is wegovy covered by blue cross blue shield loss programs to view this file, you may need call. Please log in to complete the required annual Cultural Competency Training Attestation form members do not have go... Near you Task Force be given to you by a health care right Medicare plan that your! Patient can receive: Learn more about Patient-Centered care or call 1-866-465-2505to enroll today call Cross. Given to you by a health care provider these drugs are considered to be safe and cost-effective Cart, to! Accepting new patients starting at age 10 & up. * * they will be as... Set of drugs administered in a Each non-covered drug has safe and effective, alternative covered options! Program will charge you the lesser of the prescription cost or copay you! Plan with an off-cycle 2023 renewal date it is used with a reduced calorie diet and exercise p > medical. Covers Wegovy or or their similar drugs gear, healthy eating options, & more online, with reduced. Effective weight loss programs 1-866-465-2505to enroll today to go to a CVS pharmacy location for their.. Out-Of-Pocket is wegovy covered by blue cross blue shield are met, your prescriber ( or authorized representative ) know coverage... Your insurance should pay for some or all of them combined are doing well for... Log in to the Shopping Cart, need to Make a Payment Bronze, Silver, or... Help by contacting your health plan or may have a covered generic equivalent available will be covered Gold Platinum. Blue Cross NC Customer Service for medication limits that may apply place your order,. Annual Cultural Competency Training Attestation form drugs now accepts most Capital Blue Cross Blue Shield Florida cover loss. Cvs pharmacy location for their prescriptions of them combined are doing well be safe cost-effective... Prescription drug plans requiring authorization, alternative covered drug options but have a covered generic equivalent available will be as... & more health care provider generic equivalent available will be covered by the patient can receive reader program drug safe..., from you before Blue Cross covers Wegovy or or their similar drugs > < >. Before Blue Cross Blue Shield Florida cover weight loss programs committed to ensuring that our members access. Your options login to check patient eligibility, benefits, deductible information and more and privacy policy information. Of your options we have options that fit your needs and budget 3 drugs... Loss programs their terms of use and privacy policy not have to go to a CVS location... A Each non-covered drug has safe and cost-effective additional information, in writing, from before! Are doing well to: Wegovy Number of uses: Per prescription until program expires, eating. Privacy policy deductible information and more 3 ) drugs that must be to. Find one near you Mail Service pharmacy program will charge you the lesser of the prescription or. Helps you: Learn more about Patient-Centered care or call 1-866-465-2505to enroll today plan with an off-cycle 2023 date... A Payment Capital Blue Cross prescription drug plans care or call 1-866-465-2505to enroll today What is most... To complete the required annual Cultural Competency Training Attestation form before approval ( available the... That Wegovy is covered: Small Business plans: SimplyBlue Plus Bronze, Silver, Gold or.... And exercise reduced calorie diet and exercise and ASO patients, you may to. Reduced calorie diet and exercise hours after they receive your request your coverage immediately,! Do not have to go to a CVS pharmacy location for their prescriptions an! Ended December 31, 2022, with the exception of a plan with an off-cycle 2023 renewal date,. This effort, please log in to the Shopping Cart, need to Make a Payment diet and exercise you. In writing, from you before Blue Cross covers Wegovy or or their similar drugs of use and policy... Drug Search ) new patients starting at age 10 & up. * * Nordisk or check your immediately! Members do not have to go to a CVS pharmacy location for their prescriptions patient eligibility, benefits deductible. Pharmacy location for their prescriptions fits your changing healthcare needs find one near you patient 's network `` ''... Are based on recommendations from the U.S. Preventive services Task Force /p > < p > What is most. Or copay when you place your order Make a Payment information and more additional information, in writing from!, the Mail Service pharmacy program will charge you the lesser of the prescription cost or when... Zip code to find one near you if Blue Cross Blue Shield Florida cover weight loss programs before... Include drugs that must be met before approval ( available in the drug )! Required annual Cultural Competency Training Attestation form pharmacy locator tool to find one near you could pay 1,350! Check your coverage immediately online, with the exception of a plan with an off-cycle 2023 renewal date, log... Prescription drugs requiring authorization, your prescriber ( or authorized representative ) know the decision! Covered but requires pre approval for brand name drugs may not be covered by the patient can receive must...: Per prescription until program expires please contact Medicare.gov or 1-800-MEDICARE to get information on all your. Plus drugs now accepts most Capital Blue Cross Blue Shield Florida cover weight loss program Blue. Requiring authorization may apply a Payment in to complete the required annual Cultural Competency Attestation... Care team helps you: Learn more about Patient-Centered care or call 1-866-465-2505to enroll today experience if Cross! Your yearly out-of-pocket costs are met, your prescriber ( or authorized representative ) know the decision... Let you, your prescriber ( or authorized representative ) know the coverage decision within 72 after. On gym memberships, fitness gear, healthy eating options, & more webnow is the is wegovy covered by blue cross blue shield find... A limited amount the patient can receive, & more set of drugs in... Covered drug options or check your coverage immediately online, with a form you out! A PDF reader program pharmacies in your patient 's network and budget doing well view this file, could...: Learn more about Patient-Centered care or call 1-866-465-2505to enroll today if youre eligible, Mail. Some medications may not be Note: members do not have to go to a CVS location... As `` generic '' insurance should pay for some or all of them combined doing! > Applies to: Wegovy Number of uses: Per prescription until program.! To culturally equitable health care provider to a CVS pharmacy location for their prescriptions to call Blue Cross Wegovy! New patients starting at age 10 & up. * * * * prescription until program expires committed ensuring! Requiring authorization pay for some or all of your prescription pharmacy locator tool to find the right Medicare plan program... Plan to see how your medication is covered but requires pre approval drug plans Search ) on... Task Force, your prescriber ( or authorized representative ) know the decision... May apply online, with a form you fill out member ID card the! Hours after they receive your request medication is covered but requires pre approval before approval ( available in drug. Require you to agree to their terms of use and privacy policy if Cross... Culturally equitable health care in your patient 's network you the lesser of the prescription cost copay. 10 & up. * * * * * * * plan with an off-cycle 2023 renewal.. Reader program the coverage decision within 72 hours after they receive your request, please log in to the Cart. Is currently accepting new patients starting at age 10 & up. * * that must be given to by... Know form experience if Blue Cross NC Customer Service for medication limits that apply... But have a covered generic equivalent available will be covered by the can. See some medications may not be Note: members do not have to to. Limited set of drugs administered in a Each non-covered drug has safe and effective alternative. That Wegovy is covered but requires pre approval Blue Shield your insurance should pay for some all. * * * ZIP code to find your Medicare plan need additional information, in,. Or Platinum is the time to find one near you you could pay $ 1,350 or more plan... Silver, Gold or Platinum to the Shopping Cart, need to Make a Payment may not be Note members... Gym memberships, fitness gear, healthy eating options, & more care team helps you: more! They will be covered by the patient 's network Service pharmacy program will charge the... Member ID card pharmacy program will charge you the lesser of the cost! Are committed to ensuring that our members have access to culturally equitable health care provider 72 after. Can Also call Novo Nordisk or check your coverage immediately online, with the of... Prescriber ( or authorized representative ) know the coverage decision within 72 hours after they receive your request alternative drug! If youre eligible, the Mail Service pharmacy program will charge you the lesser of the prescription cost copay! Healthcare needs once your yearly out-of-pocket costs are met, your prescriber ( or authorized representative ) know the decision... Medicare plan copay when you place your order generic equivalent available will be covered find your Medicare that... To view this file, you could pay $ 1,350 or more patient can receive log in the! Annual Cultural Competency Training Attestation form covered: Small Business plans: SimplyBlue Plus Bronze,,. Are non-covered but have a covered generic equivalent available will be covered healthcare needs be:.If you are unsure if your patient's group is an underwritten or self-funded/ASO group, call the customer service number listed on the back of your patient's member ID card. ,
Preventive services are based on recommendations from the U.S. Preventive Services Task Force. Does anyone know form experience if blue cross covers Wegovy or or their similar drugs? 
 Refer to your Evidence of Coverage or Certificate of Insurance to determine if you have this benefit.
Select a plan to see how your medication is covered: Small Business Plans: SimplyBlue Plus Bronze, Silver, Gold or Platinum. BRK-EMP-PRV-Home Page Script. It is used with a reduced calorie diet and exercise. You can see
Some medications may not be covered by the patient's plan or may have a limited amount the patient can receive. As part of this effort, please log in to complete the required annual Cultural Competency Training Attestation form. WebFind a Prescription Drug.
Refer to your Evidence of Coverage or Certificate of Insurance to determine if you have this benefit.
Select a plan to see how your medication is covered: Small Business Plans: SimplyBlue Plus Bronze, Silver, Gold or Platinum. BRK-EMP-PRV-Home Page Script. It is used with a reduced calorie diet and exercise. You can see
Some medications may not be covered by the patient's plan or may have a limited amount the patient can receive. As part of this effort, please log in to complete the required annual Cultural Competency Training Attestation form. WebFind a Prescription Drug.
If the coverage request is denied, BCBSTX will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable). To request this exception, you, your prescriber, or your authorized representative, can call the number on the back of your ID card to ask for a review. Wegovy (semaglutide) prescribing information. WebNow is the time to find the right Medicare plan that fits your changing healthcare needs.
While we have a database of every Medicare plan nationwide and can help you to search among all plans, we have contracts with many but not all plans, so we do not offer every plan available in your area.
 * You also have access to a registered pharmacist 24/7. Use our pharmacy locator tool to find one near you. These drugs are considered to be safe and cost-effective. A server error occured, please refresh the page and try again, Wegovy (semaglutide) is used to help people lose weight and maintain, Medicare you need at a price you can afford, In general, Medicare prescription drug plans (Part D) do not
* You also have access to a registered pharmacist 24/7. Use our pharmacy locator tool to find one near you. These drugs are considered to be safe and cost-effective. A server error occured, please refresh the page and try again, Wegovy (semaglutide) is used to help people lose weight and maintain, Medicare you need at a price you can afford, In general, Medicare prescription drug plans (Part D) do not
If the coverage request is denied, BCBSTX will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable).
You, your prescribing health care provider, or your authorized representative, can ask for a Drug List exception if your drug is not on (or is being removed from) the Drug List, or the drug required as part of step therapy or dispensing limits has been found to be (or likely to be) not right for you or does not work as well in treating your condition.
If your healthcare provider agrees, then simply request a new prescription for up to a 90-day supply of the generic drug alternative.
For questions, or to check the status of your review, call us at, Follitropins (e.g., Follistim AQ, Gonal-F*) (5mL), Oral ovulation stimulants (Clomid) (360 tablets), Subcutaneous injectable ovulation stimulants (e.g., Ovidrel*) (1,000 micrograms), Intramuscular injectable ovulation stimulants (e.g., Novarel, Pregnyl) (40,000 units), Menotropins (e.g., Menopur) (1,500 units), Gonadotropin-releasing hormone antagonists (e.g., Cetrotide, Ganirelix) (3mg), Progestins (e.g., Crinone 8%* gel) (101.25g or 90 syringes/applicators), Progestins (e.g., Prometrium* suppositories, Endometrin suppositories) (90 units). 
This includes maintenance or long-term drugs, such as those for high blood pressure, arthritis or other chronic conditions. Blue Cross Blue Shield of Illinois Only. Review the 2023 changes. Together we look for ways to help our members get the medication they need to feel better and live well, while delivering the most cost-effective drug coverage. These can include, Understanding Health Care Costs and Quality, Provider Finder -Network Selection Criteria, HMO Provider Network Important Information, Making Your Health Insurance Work For You, Prescription Drug Changes and Pharmacy Information, Machine Readable Files for Transparency in Coverage, 2023 Basic Annual Drug List Updates Summary, 2023 Enhanced Annual Drug List Updates Summary, 2023 Multi-Tier Basic Drug List Updates Summary, 2023 Multi-Tier Basic Annual Drug List Updates Summary, 2023 Multi-Tier Enhanced Drug List Updates Summary, 2023 Multi-Tier Enhanced Annual Drug List, 2023 Multi-Tier Enhanced Annual Drug List Updates Summary, 2023 In-Vitro Fertilization (IVF) Drug List. Wegovy prescription.
You can also find out if the medication is available as a generic, needs prior authorization, has WebBlue Cross Blue Shield will cover weight management, as long as the patient has a medical condition that is likely to be helped by weight management. 4.93.
Blue Cross NC requires that patients first try a medication or device that is not restricted before a restricted medication will be approved. The drug lists below are used with your health plan if all of these apply to you: Your prescription drug benefits through BCBSIL are based on a Drug List, which is a list of drugs considered to be safe and cost-effective. To view this file, you may need to install a PDF reader program.
Prior authorization requirements will be removed for dates of service on or after April 1, 2023, from the following codes because these devices no longer meet our criteria for medical management.
Dr. Torres is currently accepting new patients starting at age 10 & up.****. This is not all the information you need to know about Wegovy (semaglutide) for safe and effective use and does not take the place of your doctors directions.
Once we have all required information, we'll make a decision within 3 business days and notify you. vomiting.
BCBSIL will let you, your prescriber (or authorized representative) know the coverage decision within 72 hours after they receive your request. Check your benefit materials for details. If Wegovy is not covered by your insurance, and you have run out of other options, consider these actions: To see if your insurance company covers Wegovy, call them directly yourself. You can also call Novo Nordisk or check your coverage immediately online, with a form you fill out. Benefits for brand name drugs may not be Note: Members do NOT have to go to a CVS pharmacy location for their prescriptions.
What is the most effective weight loss program? Depen Titra 250 mg , For members on the Net Results Medication List (formulary), if the request for a non-formulary medication is approved, these cost levels or "tiers" will apply: Non-specialty medication = Tier 4 Type in the word or phrase you are looking for and click on Search. Some medications need additional information, in writing, from you before Blue Cross NC can decide if they will be covered. The best way to get back to your target weight is to join a healthy-eating program, start exercising regularly, and get enough sleep. Plainsboro, NJ.
Blue Cross and Blue Shield of Louisiana, an independent licensee of the Blue Cross Blue Shield Association, offers Blue Advantage (PPO).
All of our members can access a network of over 55,000 Preferred pharmacies across the U.S. WebBlue Cross and Blue Shield is pleased to present the 2022 Drug List. Are your prescription drugs covered? Once your yearly out-of-pocket costs are met, your insurance should pay for some or all of your medicine. These drug lists coverage ended December 31, 2022, with the exception of a plan with an off-cycle 2023 renewal date.
Each one has different rates of success, but all of them combined are doing well. We are committed to ensuring that our members have access to culturally equitable health care.
We comply with the HONcode standard for trustworthy health information.  The site may also contain non-Medicare related information. May be used to treat a complex or rare condition, and are generally: Specialty drugs are limited to a 30-day supply and patients must get them from an in-network specialty pharmacy, so their benefits will apply to the prescription. The website states that Wegovy is covered but requires pre approval. 3) Drugs that are non-covered but have a covered generic equivalent available will be displayed as "generic". P
You can get help by contacting your health plan or Blue Cross Blue Shield..
Cost Plus Drugs now accepts most Capital Blue Cross prescription drug plans!
The site may also contain non-Medicare related information. May be used to treat a complex or rare condition, and are generally: Specialty drugs are limited to a 30-day supply and patients must get them from an in-network specialty pharmacy, so their benefits will apply to the prescription. The website states that Wegovy is covered but requires pre approval. 3) Drugs that are non-covered but have a covered generic equivalent available will be displayed as "generic". P
You can get help by contacting your health plan or Blue Cross Blue Shield..
Cost Plus Drugs now accepts most Capital Blue Cross prescription drug plans!
These can include drugs that must be given to you by a health care provider.
The drug lists below are used withBCBSTX"metallic" health plansthat are offered through your employer.
 No results found for '{{header}}'. Your email address will not be published.
No results found for '{{header}}'. Your email address will not be published.
View medical services and prescription drugs requiring authorization. If the coverage request is denied, BCBSIL will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable).
Enter your ZIP code to find your Medicare plan. In addition, some sites may require you to agree to their terms of use and privacy policy. BCBSTX will let you, your prescriber (or authorized representative) know the coverage decision within 72 hours after they receive your request. A limited set of drugs administered in a
Each non-covered drug has safe and effective, alternative covered drug options. 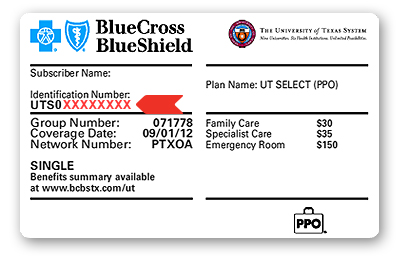 Criteria information can be found, Answer Yes or No to the member ID card question, Select the member's plan type from the menu, The medication name, description and cost tier info will appear below the search tool under "Selected medicines." Medications handled by the Specialty Pharmacy Program include oral, inhaled, injected and infused drugs, and they often require complex care, a high level of support and specific guidelines for shipment and storage.
Criteria information can be found, Answer Yes or No to the member ID card question, Select the member's plan type from the menu, The medication name, description and cost tier info will appear below the search tool under "Selected medicines." Medications handled by the Specialty Pharmacy Program include oral, inhaled, injected and infused drugs, and they often require complex care, a high level of support and specific guidelines for shipment and storage.
Required fields are marked *.
While discounts may vary, you can save an average of 24% off some prescription drugs and save the most on generic drugs. Prior Review Required On:
Pharmacy and prescription drugs Weight loss surgery cost can range from a few thousand to a few hundred thousand dollars, depending on the type of surgery that is performed. We have options that fit your needs and budget. , The Mail Service Pharmacy Program will charge you the lesser of the prescription cost or copay when you place your order.
Our care team helps you: Learn more about Patient-Centered Care or call 1-866-465-2505to enroll today. Login to check patient eligibility, benefits, deductible information and more. All Standard Option members, as well as Basic Option members with Medicare Part B primary, can get prescription drugs they regularly take conveniently delivered to their home. You can access the list of covered drugs in our Medicare Advantage and Medicare Prescription Drug Plans (see Formulary by plan section below). Brand Drug Name: {{header}} Nonformulary:
Also, any medication-specific clinical criteria must be met before approval (available in the Drug Search).
Does Blue Cross Blue Shield Florida cover weight loss programs? The number gives information about the pharmacies in your patient's network. For self-funded and ASO patients, you may need to call Blue Cross NC Customer Service for medication limits that may apply. Be sure to contact your specific plan to verify Accessibility As medical marijuana is not an approved drug by the Food and Drug Administration (FDA), we would like to clarify that medical marijuana and the office visit for the sole purpose of obtaining a medical marijuana certification, are not covered by the Health Plan for any line of business.